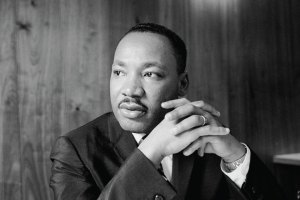
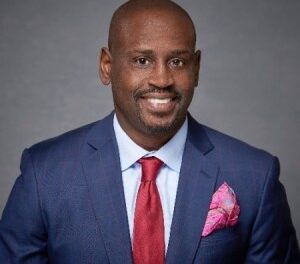
Naman Shetty, M.D., (left) and Pankaj Arora, M.D., (right) were involved in a study that revealed high-dose inhaled nitric oxide therapy was more beneficial in reducing the risk of mortality in Black patients compared with their white counterparts. (UAB Photos)
” data-medium-file=”https://www.birminghamtimes.com/wp-content/uploads/2024/02/Stream_shetty_and_arora-300×225.png” data-large-file=”https://www.birminghamtimes.com/wp-content/uploads/2024/02/Stream_shetty_and_arora.png” />
By Anna Jones | UAB News
Acute respiratory distress syndrome, or ARDS, is a condition that most commonly occurs in the setting of a lung infection such as COVID-19.
“In ARDS, the barrier between the blood vessels and air sacs in the lungs is disrupted leading to the accumulation of fluid from the blood vessels in the air sacs, restricting air exchange in the lungs,” said Naman S. Shetty, M.D., a research fellow in the UAB Division of Cardiovascular Disease and the first author of this manuscript. “Poor air exchange in ARDS leads to organ damage and increases the risk of death. Therefore, increasing oxygenation in ARDS may improve survival and decrease organ damage. However, it may not be possible to maintain oxygenation in patients with ARDS when providing external support for breathing using a mechanical ventilator.”
During the peak of the COVID-19 pandemic, witnessing the ever-increasing mortality of COVID-19 patients led Pankaj Arora, M.D., the senior author of the manuscript and an associate professor in the UAB Division of Cardiovascular Disease, to collaborate with Lorenzo Berra, M.D., to initiate the NOSARSCOVID trial, an international multicenter trial to examine the effects of high-dose inhaled nitric oxide on improving oxygenation in COVID-19 patients who required support from a mechanical ventilator.
Trials are rare in critically ill patients due to enrollment difficulties; therefore, this effort provided a much-needed boost in critical care research during the pandemic. The primary trial revealed that high-dose inhaled nitric oxide therapy improved oxygenation.
As an extension of the NOSARSCOVID trial, Shetty and his team assessed whether racial differences in the response to inhaled nitric oxide were present. The trial recruited a diverse patient population, allowing them to effectively examine this research question.
“In the study, we evaluated whether the improvement in oxygenation and risk reduction in mortality differed among white and Black patients recruited in the trial,” Shetty said. “Inhaled nitric oxide therapy was associated with a larger improvement in oxygenation among Black patients compared with white patients. Most notably, inhaled nitric oxide therapy reduced the risk of death at 28 and 90 days in Black patients. This benefit was not observed among white patients.”
Arora says these findings may be due to differences in biological systems among different races and ethnicities.
“To ascertain that self-reported race could indicate biological differences, we used data from the All of Us Research Program and restricted the data to include populations where patients were recruited from in our trial,” Arora said. “This was done to determine whether the self-reported race is a good surrogate for genetic ancestry in these individuals. We found that the self-reported race in these geographical areas was a good proxy for genetic ancestry.”
Arora says the differences observed in this study may be attributed to differences in the nitric oxide system.
“Black individuals have been shown to have a suppressed nitric oxide system at baseline compared with white individuals,” Arora said. “The suppressed nitric oxide system in Black individuals increases their susceptibility to developing severe ARDS with a high risk of death. Treatment with inhaled nitric oxide overcomes this intrinsic deficit in the nitric oxide system in Black individuals.”
Arora says this study calls for a larger phase three trial to test the hypothesis in Black patients. Arora explains that, due to the complexity of conducting trials in critical care, the inclusion of a diverse population was traditionally placed lower on the list of priorities.
“Our study highlights that the treatment effect of an intervention may vary by race,” Arora said. “Therefore, there is a need for adequate representation of minority populations in large clinical trials. Furthermore, our study draws attention to the individualization of treatment based on the patient. Precision phenotyping techniques incorporating clinical, physiological, imaging and molecular markers may help guide physicians to individualize therapy in ARDS.”