By AMANDA SEITZ Associated Press
As obesity rates rise among older adults, some lawmakers say the United States cannot afford to keep a decades-old law that prohibits Medicare from paying for new weight loss drugs, including Wegovy and Zepbound. But research shows the initial price tag of covering those drugs is so steep it could drain Medicare’s already shaky bank account.
A look at the debate around if — and how — Medicare should cover obesity drugs:
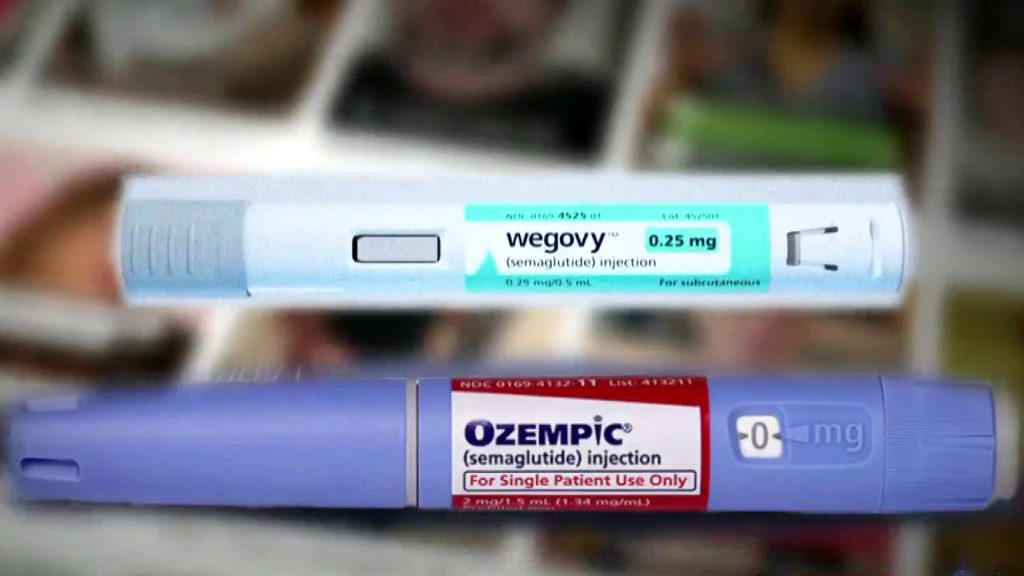
WHAT OBESITY DRUGS ARE ON THE MARKET AND HOW DO THEY WORK?
The Food and Drug Administration has in recent years approved a new class of weekly injectables, Novo Nordisk’s Wegovy and Eli Lilly’s Zepbound, to treat obesity.
People can lose as much as 15% to 25% of their body weight on the drugs, which imitate the hormones that regulate appetites by communicating fullness between the gut and brain when people eat.
The cost of the drugs, beloved by celebrities, has largely limited them to the wealthy, A monthly supply of Wegovy rings up at $1,300 and Zepbound will put you out $1,000. Shortages for the drugs have also limited the supplies. Private insurers often do not cover the medications or place strict restrictions on who can access them.
Last month, a large, international study found a 20% reduced risk of serious heart problems such as heart attacks in patients who took Wegovy.