By Mylika Scatliffe
AFRO Women’s Health Writer
Awareness of colorectal cancer might be highlighted during the month of March, but it is never far from Kelli Bagby’s mind. Her sister, Danielle Bagby succumbed to the disease in 2021.
She was 35 years old.
“Early diagnosis can make or break the outcome of a colon cancer journey,” said Bagby, of Baltimore.
According to the Centers for Disease Control and Prevention (CDC), the U.S. Preventive Services Task Force recommends adults aged 45 to 75 be screened for colorectal cancer.
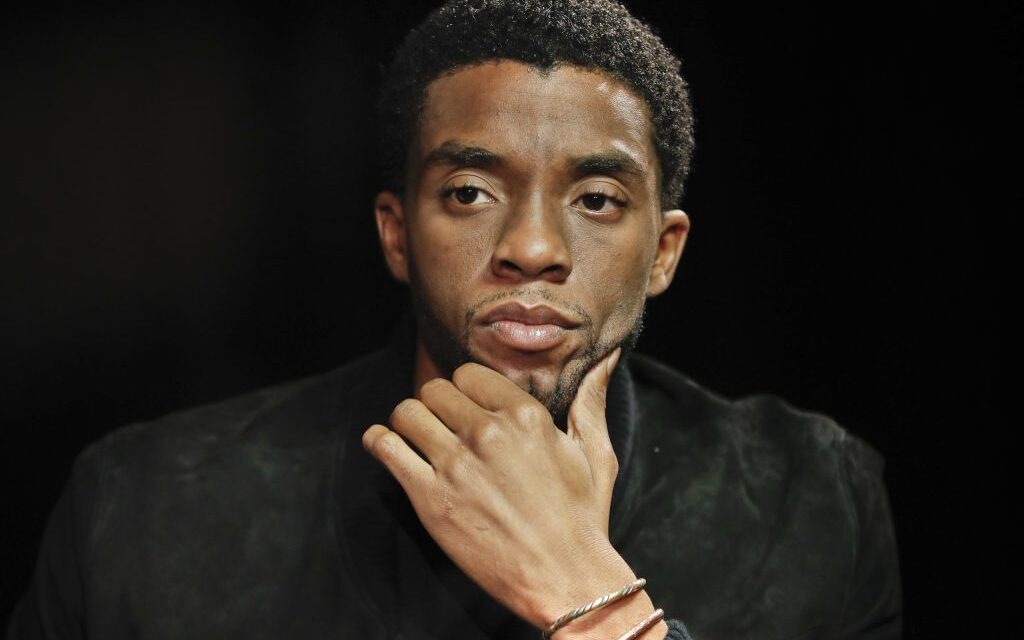
The world was dismayed when Black Panther star Chadwick Boseman died from colon cancer on August 28, 2020. The public’s shock was two-fold since Boseman never spoke publicly about his diagnosis, and he was just 43-years old when he died.

Colorectal cancer is not as common in people younger than age 50 as it is in older individuals, but it is not as uncommon as one might think. According to the American Cancer Society, in 2020 about 12 percent of colorectal cancers, or 18,000 cases, were predicted to be diagnosed in individuals under age 50 in the United States. While the rates of colorectal cancer have dropped among older groups in recent years, they have increased among younger people. It also disproportionately affects the Black community in the United States. African Americans are about 20 percent more likely to get colorectal cancer and 40 percent more likely to die from it than most other groups.
“Young people across racial lines are being diagnosed at younger ages and at a more advanced stage of the disease which contributes to their dying at earlier ages,” said Dr. Joseph DiRocco, director of gastrointestinal oncology for the Sandra and Malcolm Berman Cancer Institute at Greater Baltimore Medical Center (GBMC) in Towson, Md.
DiRocco emphasized to the AFRO that early diagnosis is crucial for a positive outcome with colon cancer.
“We’re seeing younger people with advanced progression of the disease because they are not being screened. Recommended screening for those of average risk doesn’t begin before age 45 so a colonoscopy doesn’t immediately come to the mind of a 30-year-old,” DiRocco said.
While the American Cancer Society doesn’t recommend screening before age 45 for most people of average risk, it is important for anyone of any age to recognize possible colorectal cancer symptoms. They include:
- A change in bowel habits, such as diarrhea or constipation, or narrowing of the stool that lasts more than a few days
- Needing to have a bowel movement but not feeling relief when you have one
- Rectal bleeding
- Blood in the stool, which might give the stool a dark brown or black appearance
- Abdominal pain or cramping
- Fatigue
- Losing weight with no effort
The loss of her sister created in Bagby a desire to advocate for colorectal screening as part of preventive health care, much like checks for blood pressure, cholesterol or diabetes.
“My sister was in so much pain one morning she couldn’t get off the floor. She was fine the day before. We rushed her to the emergency room where we found out she had stage IV colorectal cancer. We couldn’t believe it,” exclaimed Bagby.
She didn’t recall her sister having any symptoms out of the ordinary prior to the emergency room visit, and there was no history of colon cancer in their family. “She’d mentioned some constipation, but we just chalked that up to other things – needing to eat a little better or drink more water, but we would have known it was cancer a lot earlier if she’d had some sort of screening as part of her normal healthcare,” Bagby said.
“There may not be symptoms of colon cancer when it first develops. The incidents that are caught early are almost always discovered during colonoscopies, which most people younger than 45 aren’t having. By the time they have symptoms and get checked out, the cancer is at a later stage and may have even spread to the lymph nodes or other organs,” said DiRocco.
DiRocco also commented that while having a family history of colorectal cancer increases individual risk, many of his patients have no family history of the disease at all. There is no definitive answer as to why younger people are dying at such an increased rate.
As reported by the American Cancer Society, there are risk factors of colorectal cancer – some that can be changed and some that cannot. Lifestyle factors linked to colorectal cancer include obesity, type 2 diabetes, cooking meat at very high temperatures, a diet high in red meat, smoking and alcohol consumption.
Some risk factors over which individuals have no control include:
- Age – Colorectal cancer is more common after age 50, although it’s on the increase among people younger than 50.
- Racial and ethnic background- American Indian and Alaska Native people have the highest rates of colorectal cancer in the United States, followed by African- American men and women.
- Your sex at birth- Men are more likely to die from colorectal cancer than women.
- Gallbladder removal
- Personal history of colorectal cancer or colorectal polyps – If you have had colorectal cancer, even if it was removed, there is an increased chance of developing new cancers in other parts of the colon or rectum.
As with almost every other aspect of life for underserved communities, health disparities that affect access and quality of care influence colorectal cancer outcomes. Lack of insurance or being underinsured often means individuals lack a primary care physician to keep them on track with health screenings.
Bagby believes this was a factor in her sister’s tragic outcome.
“My sister was an entrepreneur and didn’t have high quality insurance. Maybe if she did, or if she had a primary care physician, her cancer may have been caught earlier and not at such advanced progression by the time she was diagnosed. Better insurance means better access and better quality of care, and it shouldn’t be that way. Everyone deserves quality health care,” said Bagby.
There is no discussion of colorectal cancer screening without acknowledging the stigma attached to it.
“Not many people want to talk about their poop or endure the dreaded colonoscopy,” said DiRocco.
“It’s not really the procedure that concerns people, it’s the required prep. Patients put off scheduling colonoscopies because they want to avoid it,” DiRocco continued.
There is no proven way to prevent colorectal cancer, but screenings can find abnormal, pre-cancerous cells before they develop into cancer.
Both Bagby and DiRocco agree that early screening is crucial. It can save your life.
The post Experts speak on colorectal cancer, recommend screenings at younger ages appeared first on AFRO American Newspapers.