By Pierre Vigilance, MD, MPH; Director, Health at Centri Tech
The COVID pandemic and social justice uprisings of 2020 highlighted a number of societal disparities with few more resonant than the race and socioeconomic status-based differences in the risk of contracting the illness and the risk of dying from it. But COVID can be replaced by any number of diseases and the same correlations hold true. In fact, it is the very presence of pre-COVID disparities – conditions like diabetes, asthma, chronic lung disease, and cardiovascular disease – that placed so many in Black and Brown communities squarely in the pandemic’s crosshairs. We saw the same thing with SARS in 2003, H1N1 in 2009, and now with the blinders at least partially pulled back, we have the opportunity to avoid repeating paragraphs like this when the next novel communicable disease pandemic occurs.
The opportunity is here, the question is: Do we have the appetite to make the shifts in policies, programs, platforms, and products necessary to prevent repeated insults and unnecessary deaths?
Part of the answer to that question lies in our collective desire to work across sectors and silos, and to share accountability for the multidirectional cause:effect relationships that intersect in our daily lives. One key intersection is between health and education.
Most commentary about this junction is aimed at the impact that improving education has on health. This is based on the assertion that the better one’s education, the more socially mobile we become, allowing participation in markets where better income, housing, job security, etc. create the foundation for potentially less stressful living environments, better access to services, more self-agency, and longer, healthier lives. But what impact does health have on education outcomes?
Chronic diseases contracted early in life and adverse childhood experiences both play a role in educational attainment[1] and therefore impact income which is a key determinant of health. A comprehensive response to our question needs to go beyond diseases and into the social determinants of health.
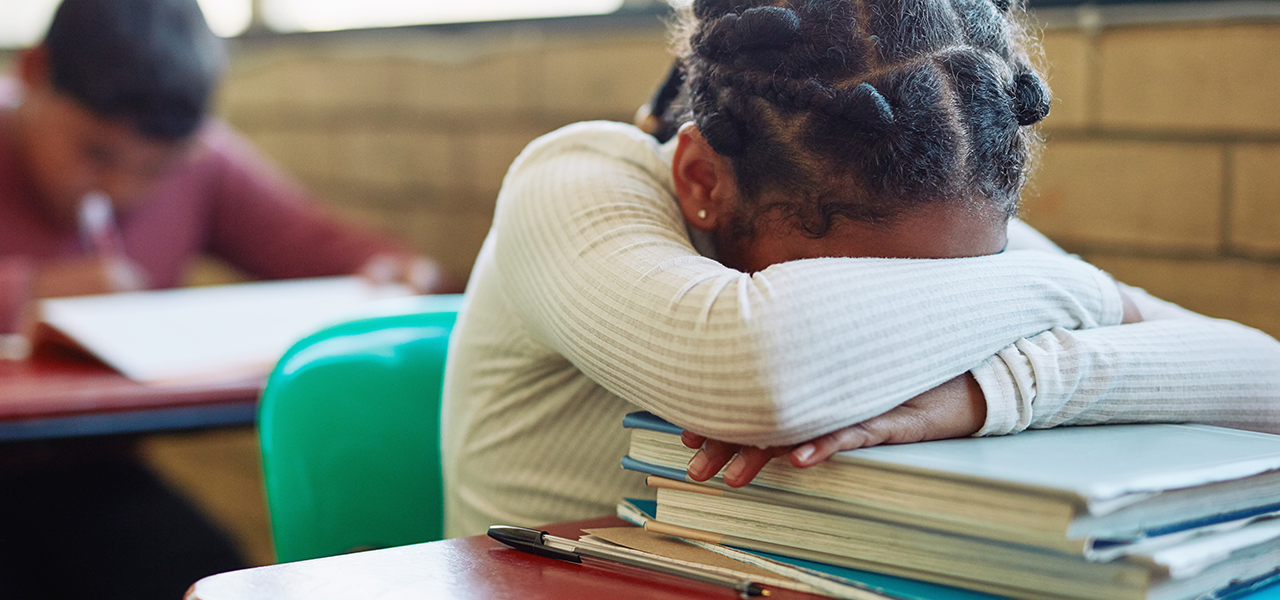
Take food security for example – being motivated to learn is not unlike being motivated to exercise in that it helps to be well-prepared, and food plays a major role. Missing meals (particularly breakfast) impacts a student’s ability to concentrate. Foods that cause spikes and crashes in blood sugar levels challenge a student’s ability to maintain the level of concentration and awakeness needed to participate and thrive in class. Another example is housing: it provides a place for comfort and sleep, but only if it is quiet and safe. Children deprived of sleep are unable to function during the school day, making them less able to learn, and potentially more likely to act in a way that might inaccurately suggest a psychological frailty.
Living in a home or community that is perpetually noisy, challenges the time young minds need to recover and grow. It is just as important to screen for these factors as it is for every child to have an annual physical exam. That exam should assess them comprehensively, arm parents with the information they need to address issues and remove any barriers to school engagement. Part of that physical should be routine vision and hearing exams, as deficits in these systems have significant impact or are often taken for granted and possibly not assessed. Having a provider-relationship also gives parents access to a trusted voice they can turn to when they have questions about their child’s conditions, which can influence decision-making on health matters and in turn impact education statistics like absenteeism.
Another point of health:education intersection is demonstrated by the manner in which young people in particular have been affected by COVID. With record rates of mental health and other health-related issues reported in a number of vulnerable populations, the pandemic is destined to have long term effects beyond our immediate view. The increase in youth disconnection[2] during the pandemic is cause for concern with post-secondary education enrollment impacted most significantly in community colleges – which traditionally serve under-represented minorities and low-income students.
The already fragile bridge from high school to college was further impacted by the economic, social, and psychological impact of the pandemic. And this has impacted the workplace as well, where similar increases in disconnection have been noted for young adults[3], leaving them out of work, out of school, and more prone to even greater detachment.
Some of this disconnectedness is related to the slow progress we have collectively made towards digital inclusion – the ability for people to be able to access, adopt, sustainably use, and receive value from engagement with digital tools. Broadband access is increasingly being recognized as an essential utility and a social determinant of health[4], and this is for good reason. With so many social, financial, educational, and communication needs met by digital services, the pursuit and maintenance of health is significantly impacted by access to the digital economy and the digital tools needed to engage in it. And the ability to access resources, everything from food and education to medication, disease management, and time with a provider, all rides (or soon will) on access to perpetually affordable, and meaningful bandwidth broadband connectivity alongside up-to-date hardware. This is where the social determinants impacting health can be addressed, improving health outcomes, creating greater readiness to learn and the closure of a feedback loop with ever-diminishing barriers to access and the eventual achievement of health equity.
Income and race-related disparities in health outcomes correlate with the lack of digital access, and while government programs established to address this have been launched, the awareness and adoption of these programs is relatively limited. Many potential institutional partners speak to their expectation that underserved populations participate in government-sponsored programs, but we have seen little appetite for piloting scalable local broadband access solutions that might support the future adoption of government sponsored programs. Because of the multi-sector impact of improved broadband access, no one sector should be responsible for infrastructure investments in this area. Cross-sector coalitions aligned on the value of improved health and educational outcomes should be formed alongside government agencies, i.e. health, education, housing, and employment services to drive improvements in health and consequently education, to catalyze all the downstream benefits that follow.
[1] Impact of health & circumstance on education
[4] Broadband as essential infrastructure
The post COMMENTARY: Health’s Impact on Education appeared first on NNPA Education Public Awareness Program.