By Mike Cason
A bill to expand Alabama’s screening of newborns for rare diseases, which is vital for early intervention and treatment that can lengthen and improve the quality of lives, has become law thanks to an outgoing 15-year-old from Foley, his family and a grassroots organization.
The Zachary Thomas Newborn Screening Act, named after the teenage advocate, will add to the list of diseases infants are tested for in Alabama and is intended to align the state’s program with the federal Recommended Uniform Screening Panel (RUSP), which adds diseases periodically.
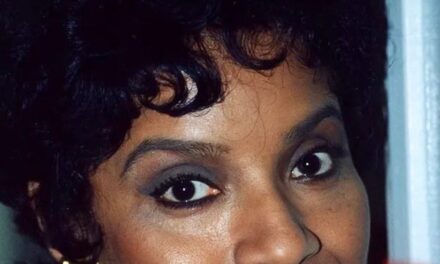
Zachary’s mother, Brooke Thomas, said he is a patriotic history buff and a natural when it comes to working the halls at the Alabama State House, shaking hands, and building good will for their cause.
“He just wants to help people,” Thomas said. “And we were able to kind of convey to him that our family, we don’t fight for newborn screening for us. But we do this for the families that we haven’t met yet.”
“He loves thinking that he’s helped a baby somewhere,” said Brooke Thomas, chief programs officer for Alabama Rare, which advocates for families affected by rare diseases.
Alabama tests for 33 of the the 37 primary diseases on the federal RUSP. Zachary was diagnosed at age 1 with one of the four that is not on Alabama’s list – MPS I. People with MPS I, also known as Hurler syndrome, do not produce an enzyme needed to break down certain complex sugars. Those sugars accumulate in the body, causing a wide range of damage and developmental problems.
Zachary’s sister Amelia, 12, and brother Luke, 8, also have Hurler syndrome. Enzyme infusions and stem cell transplants can slow the progression and damage. Like many other diseases on the RUSP, starting those treatments early is vital.
Rep. Phillip Rigsby, R-Huntsville, sponsored HB77, the bill named after Zachary, which passed the House and Senate without a dissenting vote and was signed into law by Gov. Kay Ivey.
“The issue with these diseases is we have treatments for a lot of them, but they’re most effective if you catch it very early on, which is why the newborn screening is so important,” Rigsby said. “The further the treatment is delayed, the shorter the benefit, or, shorter the lifespan expansion that you’re going to receive from that treatment.”
Rigsby, a pharmacist who was elected to the House in 2022, said Alabama Rare, an advocacy organization founded by Swapna Kakani of Huntsville, approached him about the legislation. He attended a breakfast to learn more about the issues and met Zachary and Brooke Thomas. The Alabama Department of Public Health (ADPH) worked with Alabama Rare to develop the bill.
The Alabama Newborn Screening Program tests every infant, although parents can opt out. The screening includes a small heel prick usually done when babies are in the nursery after delivery, said Dr. Wes Stubblefield, a pediatrician and medical officer for the Alabama Department of Public Health. The blood is placed on a special kind of filter paper that goes to the Alabama Bureau of Clinical Laboratories in Prattville.
About 60,000 babies a year are tested through the program. The tests annually identify about 200 babies who have a congenital disorder. Most look and act healthy at birth. In addition to the heel prick, the state’s screening program checks for hearing loss and for congenital heart problems using a pulse oximeter, Stubblefield said.
Stubblefield said the heel prick is generally repeated by pediatricians during an infant’s office visit about two weeks after birth.
The RUSP includes many diseases that are unfamiliar to most people, like MPS I, but also more well known conditions such as sickle cell and cystic fibrosis.
For infants whose tests indicate an abnormality, Stubblefield said the Alabama Newborn Screening Program refers families to specialists who determine the best course of intervention and treatment, a process that often starts with another test to confirm the diagnosis.
Newborn screening started in the 1960s. Stubblefield said the earliest screens, for phenylketonuria, or PKU, and congenital hypothyroidism, are great examples of the value of the tests. Both conditions are fully treatable but result in irreversible brain damage if not detected.
“Some of these conditions require things like a bone marrow transplant, to have any hope for having a normal life,” Stubblefield said. “And the longer it takes to diagnose these conditions, the more damage is being done to the body.”
Stubblefield, who worked in private practice as a pediatrician for 14 years in Auburn and in the Shoals before moving into public health service, said it is extremely difficult for pediatricians to diagnose diseases that affect a tiny portion of the population.
”You may only see a few children in your career that have some of these very rare conditions,” Stubblefield said.
Parents who are worried that their baby has an undiagnosed condition typically can endure months of anguish seeking answers, Stubblefield said, a process that he said is often called a diagnostic odyssey.
“They know something’s not right, and they get referred around to different people, and finally the right test gets done but by then there’s irreversible damage,” Stubblefield said.
Thomas and her husband, Mich, were living in Arkansas when they went through their diagnostic odyssey with Zachary.
“It’s life changing,” she said. “I really can’t put it into words if you haven’t been there.”
She said they were fortunate that Zachary’s pediatrician was familiar with MPS I, so the diagnosis came sooner than it might have otherwise, when Zachary was 1. The doctor cautioned her not to do a Google search about MPS I.
“So naturally, that’s what you do, right?” Brooke Thomas said. The information she found at that time, 14 years ago, was bleak. For example, she learned that MPS I had previously been called gargoylism because of some of the physical traits it can cause.
Thomas said her family did what she has learned many others facing a devastating diagnosis do. They found the best course of treatment for Zachary and later for Amelia and Luke. And they connected with others for support, understanding, and inspiration to fight for a greater cause.
Zachary, Amelia and Luke received enzyme infusion therapy and stem cell transplants to treat their MPS I. Thomas said they see about 15 specialists and their care is managed by a team at the University of Minnesota at a hospital that is classified as a rare disease center of excellence. The children still face complications and long-term uncertainties. But Brooke Thomas said when she speaks to groups she always makes the point that the disease does not define her children.
Zachary likes basketball, football, Legos, Minecraft, and history and hates broccoli. Amelia likes art, music, and baking and hates broccoli. Luke, the 8-year-old, is “the king of whatever room he walks into,” his mother says, loves Pokemon and Legos and hates broccoli.
“They’ve endured more than anybody can fathom in their lives,” their mother said. “And they deal with chronic pain and these major orthopedic surgeries. But despite all that, they’re still just kids at the end of the day that hate broccoli. Everybody’s kid hates broccoli. That’s who they are. At the end of the day, they’re still just a kid.
“And their life has value. If you let them, they’ll teach you more than you could learn at any institution or through any hands-on learning experience, if you just allow families and kids like mine to show you a different perspective.”

Brooke Thomas tells other parents facing a rare disease diagnosis that the road ahead is difficult but rewarding.
“I always tell people, your life will look very different than how you’ve imagined it,” she said. “And it’s OK to take that time to grieve that. And definitely, as soon as you are able to, to get help and to talk through that.
“But this journey will take you to so many amazing places that you would never get to do,” she said.
For example, she said they stay at Ronald McDonald Houses across the country and are amazed by the love of “people who devote their lives, the scientists, our researchers, our doctors that truly care about our kids.”
“You have to grieve first,” Brooke Thomas said. “And then you have to be open to allowing that to happen.”
Stubblefield said the Alabama Newborn Screening Program and Bureau of Clinical Laboratories is preparing to add the screening for MPS I in August, as well as screening for Pompe disease, another rare genetic disorder that’s on the RUSP.
Those two additions will leave two of the primary diseases on the RUSP – MPS II and GAMT – to add later and bring the state list up to the full 37 on the federal list. Stubblefield said the program is in the research stage for adding those two.
Stubblefield said adding a disease to the screening list is a years-long process that takes staffing, equipment, and training. He said the lab has dedicated employees but has challenges in maintaining the necessary staffing levels. He said there is a need for competitive salaries, an issue he said the Legislature might have to revisit.
As more diseases are added to the federal list, HB77 calls for those to go on the state list within three years. If not, the law requires the state health officer to write a report explaining why.
“The Bureau of Clinical Laboratories is doing their absolute best to get these added as quickly as possible,” Stubblefield said. “Understanding that more will be added in the future and being at least on parity with the RUSP is vitally important to to making sure that we have a complete newborn screening program in Alabama.”
Brooke Thomas said her family’s work with Alabama Rare and advocacy will continue because it is essential.
“What we’ve learned in working and reaching out to people in other states, it’s the patients and families that really drive these kinds of policies,” she said. “And we recognize the privilege that we have. I recognize the privilege that my children are stable enough that I can devote this time, and Zachary and I can devote this time to doing this work. We definitely do this to help the friends we haven’t met yet. That’s what we always like to say.”
It helps their cause that Zachary carries an enthusiasm and a natural aptitude for making friends .
“He loves to go around and shake hands at the State House and honestly, he’s way better at it than I am,” Brooke Thomas said. “They like him up there way more than they like me.
“He was born that way. He’s gonna go around and shake hands and he’s gonna learn everybody’s name.”
During one of their trips to Montgomery, Thomas pointed out to Zachary, the history buff, where the Rev. Martin Luther King Jr., led voting rights marchers up Dexter Avenue to the Capitol in 1965.
“He was quiet for a little while,” his mother said. “And he was like, ‘Mom, would you call Dr. King an advocate?’ I was like, ‘Absolutely, yeah. He was advocating for what he believed in for marginalized people just like we do for people with disabilities and rare diseases.’ And he said, ‘I really think I like feeling like I’m doing something like Dr. King did.’”
“I’m just crying thinking about it,” Brooke Thomas said. “Like wow, this amazing kid. I don’t know where you came from, but I’m so proud of you.”